Also known as adhesive capsulitis, frozen shoulder is an inflammatory condition typified by pain and stiffness with no other obvious injury. This term is occasionally applied to any painful condition of the shoulder – which can cause confusion among patients regarding the course, treatment and expected outcome of their shoulder
Frozen shoulder is considered to be “self limiting”, that is it tends to resolve naturally over time – but this may be a very long and frustrating time! Help can be provided during this time
Frozen shoulder:
- affects people between the ages of 40-70, females more than males.
- People with diabetes are prone to it. Diabetics tend to take longer to resolve and are more likely to be left with residual stiffness.
- It is also associated with thyroid dysfunction, previous breast or lung surgery. It can occur following prolonged immobilisation or surgery on the shoulder but usually there is no identifiable cause.
- There is a 2-3x increased increased risk in twins: suggesting a genetic component
It rarely recurs in the same shouder, but there is a 20% risk of it occurring in the other shoulder. - The underlying pathology is inflammation, thickening and contracture of the shoulder joint capsule.
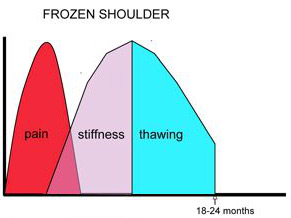
There are three phases:
- Painful phase: The shoulder gradually becomes painful for no apparent reason. It can be difficult to sleep. The chronic ache may last for 6 months (there about). Treatment during this time involves anti-inflammatory medications and a cortico-steroid injection into the shoulder to settle the inflammation.
- Stiffening phase: Movement of the shoulder is severly limited in all directions. Trying to force movement (such as with your other arm or a therapist) is not helpful and tends to make things worse. The chronic ache settles but sudden movements (such as trying to catch a falling plate) cause sharp pain. The muscles around the shoulder blade start to compensate which may lead to aching of the neck or upper back late in the day.
- Thawing phase: The stiffness slowly begins to resolve around the 12 month mark. Some people (especially diabetics) may take longer. Around 10-15% of people may have some residual loss of movement.
As the natural history is for recovery of movement and return to having a functional shoulder with no specific intervention then treatment is usually non operative. For the minority that have residual stiffness which is not improving after 12 months, surgery may be performed to resect a portion of the thickened capsule and thereby restore movement. This keyhole procedure is performed as day surgery.